Ever had a case with a foreign body in the foot? Do you know how painful this is?! 22 yo patient sent in from clinic because he had accidentally stepped on a broken wine glass several days before. The clinic removed some of the glass a few days before but returned because of ongoing pain. Here is his x-ray from the clinic.
In this case the glass is radio-opaque with a few pieces present. The patient wanted to be knocked out for this because of the amount of pain trying to remove the glass last time. The first task is to locate the glass. Seem pretty easy, right?
The glass FB on the still image is hyperechoic and causes a shadow and/or reverberation artifact. It has been highlighted on the still image, but watch the video...
A step off pad would have enhanced the visualization and detection of the foreign body. This can be done simply by using about 1 cm thickness of gel and suspending the transducer in the gel above the area of interest or getting a mini-bag of saline and scanning through that.
Next step ... removal...
Local anesthetic in this area is still extremely painful. Other options include procedural sedation and analgesia or a local block. These can be done blind, but studies have shown more effective blocks under direct visualization with ultrasound are more effective ...
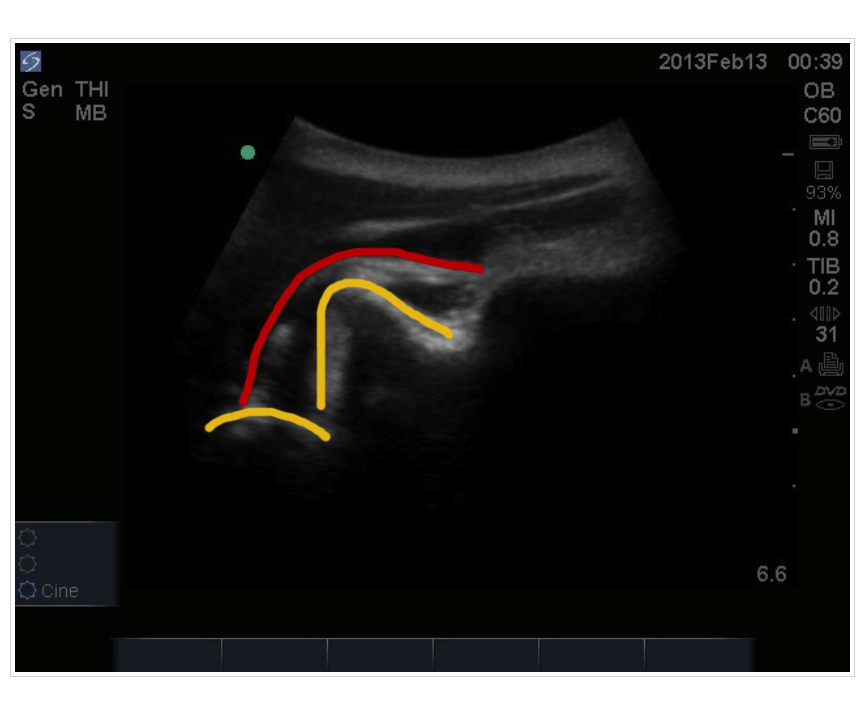
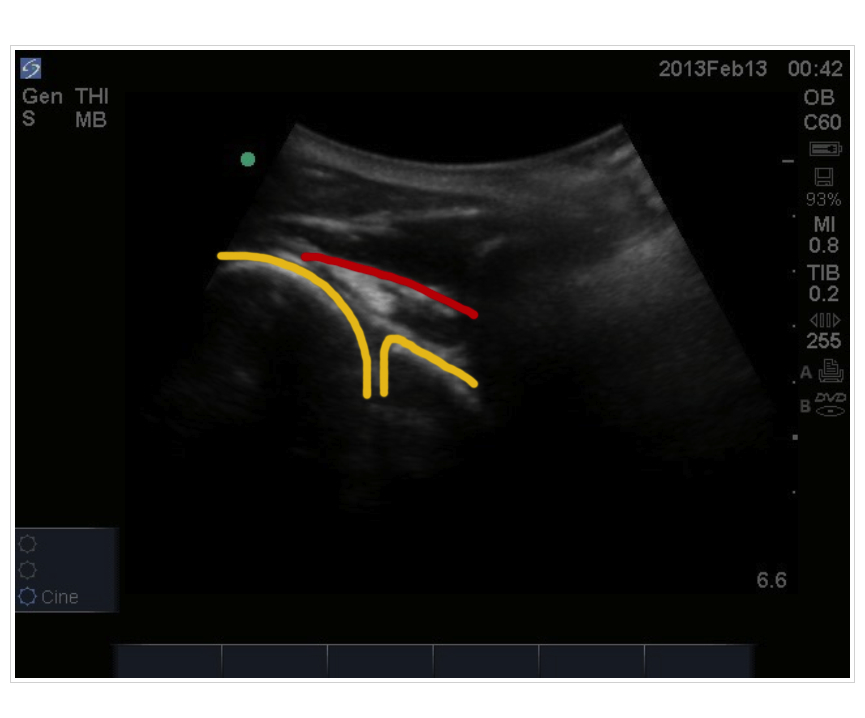
The posterior tibial nerve covers the heel completely so all you need to do is block this nerve as opposed to a complete ankle block. The anatomy is shown above. The transducer is placed just above the medial malleolus and vessels and the PTN can be visualized.
Informed consent must be obtained and should include that lidocaine will last about 5-8 hours. Lidocaine WITHOUT epinephrine is used. During this time NO weight bearing should occur for the risk of stepping on something else as well as the risk of falls. Comparisons can be made with dental freezing and no chewing because the risk of gnawing off your cheek!! All patients are discharged with crutches.
In the cine clip above, Dr. Vakani (our very own emerg resident) has advanced the needle towards the PTN avoiding the vessels. The needle can be seen coming from the left of the screen.
You can see now that the PTN is easily visualized by its honeycomb appearance as it is bathed around with lidocaine. As the needle is withdrawn, lidocaine is seen injected just above the fascia which would have resulted in a poor block if this was the only area where the lidocaine was injected.
Piece of cake? ... Not so fast .... Even though you know where the foreign body is AND you have great analgesia ... searching for these is still like a needle in the haystack. Give yourself a time limit ... 30 minutes maximum and consider calling in a consultant if it takes more time than this to do.
Hooray!! Everyone's happy right? .....
Nothing is 100% ... knowing that the foreign body in this case is radio-opaque the patient was sent back for repeat x-rays which demonstrated residual glass in the heel. A repeat ultrasound may have less utility because with dissection air is often introduced which makes the accuracy of ultrasound to pick up foreign bodies limited. The patient was subsequently referred to orthopedics who then removed the remaining foreign bodies.
In summary:
1. Consider ultrasound guided regional nerve blocks for analgesia
2. Be sure to advise of all the risks and duration of the block to the patient
3. When removing foreign bodies:
- give yourself a time limit
- you may not get everything out even though you think you have (advise the patient accordingly before you start)
Great resources:
Thank you to the patient who kindly consented for us to put this case up as well as Dr. Vakani for letting me tag along! Please feel free to provide any feedback.
Yeah ultrasound!!





 Before (glenoid and humeral head in yellow, supraspinatus tendon in red)
Before (glenoid and humeral head in yellow, supraspinatus tendon in red)